Can Other Foot Problems Cause Plantar Fasciitis?
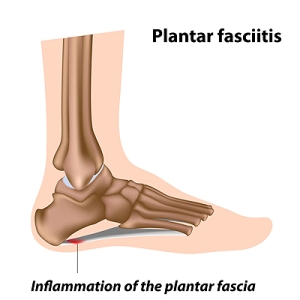
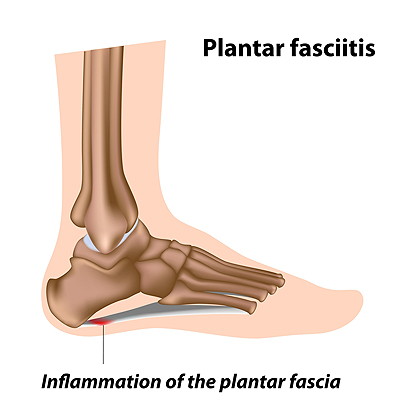
Plantar fasciitis is a condition characterized by inflammation of the plantar fascia, a ligament that runs along the bottom of the foot and connects the toes to the heel bone. This ailment is characterized by a sharp, stabbing heel pain that is at its worst when taking your first few steps after resting. There may also be pain along the arch of the foot. Although plantar fasciitis is an overuse injury often caused by repetitive movements that put excess strain on the ligament, having other foot conditions can make developing plantar fasciitis more likely. Problems such as heel spurs, abnormal foot biomechanics, flat feet, high arches, and arthritis can all impact your risk of getting plantar fasciitis. If you are experiencing the symptoms of this condition, please seek the care of a podiatrist.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Gradually Increasing Speed and Mileage May Help to Prevent Running Injuries
 People who enjoy running may overlook foot pain, which in turn can develop into serious foot conditions. Research has indicated it is beneficial to practice proper warm-up and cool down routines, as this may be helpful in preventing running injuries. Patients who are new to the sport of running are advised to start slowly, and gradually increase their speed and mileage. Additionally, it is beneficial to alternate running shoes, which may be helpful in prolonging shock absorption. If you would like more information about how running injuries can affect the feet and how to prevent them, please consult with a podiatrist.
People who enjoy running may overlook foot pain, which in turn can develop into serious foot conditions. Research has indicated it is beneficial to practice proper warm-up and cool down routines, as this may be helpful in preventing running injuries. Patients who are new to the sport of running are advised to start slowly, and gradually increase their speed and mileage. Additionally, it is beneficial to alternate running shoes, which may be helpful in prolonging shock absorption. If you would like more information about how running injuries can affect the feet and how to prevent them, please consult with a podiatrist.
All runners should take extra precaution when trying to avoid injury. If you have any concerns about your feet, contact one of our podiatrists of Pennsylvania. Our doctors will treat your foot and ankle needs.
How to Prevent Running Injuries
There are a lot of mistakes a runner can make prior to a workout that can induce injury. A lot of athletes tend to overstretch before running, instead of saving those workouts for a post-run routine. Deep lunges and hand-to-toe hamstring pulls should be performed after a workout instead of during a warmup. Another common mistake is jumping into an intense routine before your body is physically prepared for it. You should try to ease your way into long-distance running instead of forcing yourself to rush into it.
More Tips for Preventing Injury
- Incorporate Strength Training into Workouts - This will help improve the body’s overall athleticism
- Improve and Maintain Your Flexibility – Stretching everyday will help improve overall performance
- “Warm Up” Before Running and “Cool Down” Afterward – A warm up of 5-10 minutes helps get rid of lactic acid in the muscles and prevents delayed muscle soreness
- Cross-Training is Crucial
- Wear Proper Running Shoes
- Have a Formal Gait Analysis – Poor biomechanics can easily cause injury
If you have any questions, please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Prevent Running Injuries
Overtraining and overusing the feet are the main causes of common running injuries. A number of these common injuries are caused by overrunning. Runner’s knee is a condition that is characterized by the back of the kneecap beginning to wear away and cause pain in the knee. This frequently occurs due to either a decrease in strength in the quadriceps muscles or ill-fitting shoes that are lacking in proper support for the inside of the forefoot. Strengthening exercises focusing on the quad muscle and sports orthotics are the usual treatments for those suffering from runner’s knee. Prevention of the condition lies in a focus on hip strengthening and quad-strengthening to keep the kneecap aligned. To help learn the best exercise to heal runner’s knee, one can also undergo physical therapy.
One common injury, called iliotibial band syndrome, is often caused by overtraining. This condition occurs when the iliotibial band gets irritated, creating pain and discomfort in the outside knee area. Plantar fasciitis, another common running injury, also occurs as a result of inflammation and irritation. Plantar fasciitis is an inflammation and irritation of the bone in the foot. A large amount of pain is often experienced due to plantar fasciitis. The condition can be caused by a high arch, improper footwear, tight muscles, or flat feet. It can best be avoided by stretching and wearing appropriate footwear that supports the foot.
Another common injury for runners is stress fractures. These injuries occur due to running style, overtraining, or a lack of calcium. Stress fractures most often occur in several locations in runners, including the inner bone of the leg, the thighbone, the bone at the base of the spine and the bones of the toes. Stress fractures are best prevented by wearing proper footwear and by running on flat and hard surfaces; this will absorb some of the shock created during running.
Aside from overtraining, other causes of common running injuries include ill-fitting footwear, a lack of flexibility and strength, and irregular biomechanics. The best way to avoid running injuries is to prevent them from even occurring. Both iliotibial band syndrome and stress fractures are preventable. The first step that should be taken to prevent running injuries is to only wear footwear that fits properly and that is appropriate for whatever activity you are doing. Running shoes are the only protective gear available to runners that can safeguard them from sustaining injuries. Choosing the right pair of shoes is therefore extremely important. While running shoes are an important factor, it is also important to consider other facets of your running routine such as training schedules, flexibility, and strengthening. These elements should be considered and altered according to your running needs to best maximize your run and minimize the possibility of injury. Careful stretching before and after a run should also be considered to help prevent running injuries. Stretching muscles enables greater flexibility and a lesser chance of sustaining injury.
Why Do I Need an Ankle-Brachial Index Test?
 The Ankle-Brachial Index (ABI) test is a simple, fast, and noninvasive screening tool used to detect peripheral artery disease (PAD), a condition that causes poor circulation in the lower limbs. A doctor may suggest that you undergo an ABI test if you are at risk for or have symptoms of PAD. People who are older than 70, have diabetes, high lipid levels, smoke, or have abnormal pulses in their legs can have an increased risk of developing PAD. While usually asymptomatic in its earliest stages, PAD can progressively worsen and cause leg pain, cramps, and numbness, among other symptoms. An ABI test is done by measuring the blood pressure at your arm and at your ankle using a blood pressure cuff. The two numbers are then compared to each other to determine your risk of PAD. For more information about PAD, please consult with a podiatrist.
The Ankle-Brachial Index (ABI) test is a simple, fast, and noninvasive screening tool used to detect peripheral artery disease (PAD), a condition that causes poor circulation in the lower limbs. A doctor may suggest that you undergo an ABI test if you are at risk for or have symptoms of PAD. People who are older than 70, have diabetes, high lipid levels, smoke, or have abnormal pulses in their legs can have an increased risk of developing PAD. While usually asymptomatic in its earliest stages, PAD can progressively worsen and cause leg pain, cramps, and numbness, among other symptoms. An ABI test is done by measuring the blood pressure at your arm and at your ankle using a blood pressure cuff. The two numbers are then compared to each other to determine your risk of PAD. For more information about PAD, please consult with a podiatrist.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with one of our podiatrists from Pennsylvania. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Vascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.
How Feet May Show Early Warning Signs of Diabetes
According to The National Diabetes Statistics Report of 2020, over 34 million Americans over the age of 18 had diabetes in 2018. However, 7.3 million of those people were either not aware they had diabetes or did not report it. It is important to be properly diagnosed and treated for diabetes promptly as this chronic disorder causes elevated blood sugar levels which can lead to several negative health conditions throughout the body—including diabetic foot problems due to poor circulation and nerve damage. Your feet can often present warning signs of diabetes such as numbness in your toes or feet, tingling, burning, swelling, lack of feeling, or change of skin color in your feet, open sores that won’t heal, ankle pain, and more. If you notice any of these symptoms or are experiencing any pain in your feet or ankles, it is suggested that you contact a podiatrist for a thorough examination and proper diagnosis.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
What Can I Eat if I Have Gout?
 Gout is a type of arthritis that is caused by a buildup of uric acid in the bloodstream. When uric acid deposits in the joints, it crystallizes and causes symptoms such as pain, swelling, and inflammation. Gout frequently affects the joints of the feet, and specifically the big toe joint. This condition can sometimes be managed by modifying your diet. Foods that are high in purines, such as red meat, can cause the body to produce more uric acid. Therefore, their consumption should be limited. Instead, opt for foods that are low in purines, such as green vegetables, fruits, nuts, dairy products, and eggs. If you experience frequent gout flare ups, please consult with a podiatrist who can help treat and manage this condition.
Gout is a type of arthritis that is caused by a buildup of uric acid in the bloodstream. When uric acid deposits in the joints, it crystallizes and causes symptoms such as pain, swelling, and inflammation. Gout frequently affects the joints of the feet, and specifically the big toe joint. This condition can sometimes be managed by modifying your diet. Foods that are high in purines, such as red meat, can cause the body to produce more uric acid. Therefore, their consumption should be limited. Instead, opt for foods that are low in purines, such as green vegetables, fruits, nuts, dairy products, and eggs. If you experience frequent gout flare ups, please consult with a podiatrist who can help treat and manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Pennsylvania. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.