Blog
What Is Achilles Tendonitis?
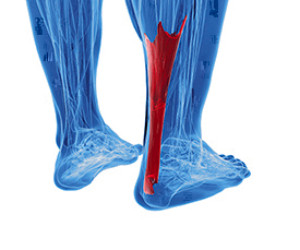 The large tendon on the back of the ankle which connects the calf muscles to the heel bone is known as the Achilles tendon. When this tendon becomes inflamed or degenerates, Achilles tendonitis can occur, which is also referred to as Achilles tendinopathy. This type of injury usually occurs due to overuse. Common factors that can contribute to the development of this condition may include poor foot biomechanics, improper footwear, wearing high heels, and over training. Patients who are noticing pain, stiffness, or tenderness in their Achilles tendon should consult with a podiatrist as soon as possible since Achilles tendonitis is easier to treat when diagnosed early.
The large tendon on the back of the ankle which connects the calf muscles to the heel bone is known as the Achilles tendon. When this tendon becomes inflamed or degenerates, Achilles tendonitis can occur, which is also referred to as Achilles tendinopathy. This type of injury usually occurs due to overuse. Common factors that can contribute to the development of this condition may include poor foot biomechanics, improper footwear, wearing high heels, and over training. Patients who are noticing pain, stiffness, or tenderness in their Achilles tendon should consult with a podiatrist as soon as possible since Achilles tendonitis is easier to treat when diagnosed early.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Lessen the Impact of High Heels on Your Feet
If you love high heels, you should be aware that wearing them regularly can take a toll on your feet and may lead to conditions like hammertoes, corns, bunions, Morton’s neuroma, plantar fasciitis, Haglund's deformity (pump bump), and more. While it may be difficult to completely kick the high heel habit, you can lessen their impact and help protect your feet. Take the heels off whenever you can throughout the day and stretch your feet. Alternate heels with flats every other day. Choose shoes that are well made and comfortable with a padded sole. Instead of slip-on, or open back high heels, wear shoes that cover more of your foot and cradle them more securely. Make sure they fit properly both in length and width. Heels that are lower are better, as are wider heels which help distribute weight more evenly. Additionally, a podiatrist may provide custom orthotics to help alleviate pressure points and provide cushion and support where it is needed. A podiatrist may also help you prevent a developing foot condition from worsening, or treat one that has already occurred.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact one of our podiatrists from Pennsylvania. Our doctors can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Is Foot Drop?
 Foot drop is often caused by a compression of the nerve that controls the muscles that lift the foot. When this occurs the front part of the foot and toes are difficult to lift or move due to muscular weakness or paralysis. Foot drop may also cause the foot to drag on the ground while walking. This is usually a sign of an underlying problem such as muscular damage, nerve damage like neuropathy, or a brain or spinal injury. While foot drop usually only affects one foot, it can affect both feet depending on the cause. It is most commonly temporary, but in severe cases it may be permanent. People who are finding it difficult to lift the front part of their foot off the ground should consult with a podiatrist who can help diagnose the underlying condition. A podiatrist will also be able to prescribe custom made orthotics or shoe inserts as well as other treatment options depending on the severity.
Foot drop is often caused by a compression of the nerve that controls the muscles that lift the foot. When this occurs the front part of the foot and toes are difficult to lift or move due to muscular weakness or paralysis. Foot drop may also cause the foot to drag on the ground while walking. This is usually a sign of an underlying problem such as muscular damage, nerve damage like neuropathy, or a brain or spinal injury. While foot drop usually only affects one foot, it can affect both feet depending on the cause. It is most commonly temporary, but in severe cases it may be permanent. People who are finding it difficult to lift the front part of their foot off the ground should consult with a podiatrist who can help diagnose the underlying condition. A podiatrist will also be able to prescribe custom made orthotics or shoe inserts as well as other treatment options depending on the severity.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact one of our podiatrists from Pennsylvania. Our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact one of our offices located in Plymouth Meeting and Ambler, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.